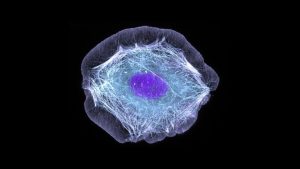
Our skin is a natural wonder of bioengineering.
The largest organ in the body, it’s a waterproof defense system that protects against infections. It’s packed with sweat glands that keep us cool in soaring temperatures. It can take a serious beating—sunburns, scratches and scrapes, cooking oil splatters, and other accidents in daily life—but rapidly regenerates. Sure, there may be lasting scars, but signs of lesser damage eventually fade away.